Planning to Develop Custom Healthcare Software?
Turn your vision into a secure, scalable, and compliant solution..
Why Custom Healthcare Software Development Matters
If you’re aiming to develop a service that meaningfully improves healthcare outcomes, opting for custom healthcare software development is an excellent choice. Generic platforms may claim to handle multiple functionalities, but they’re often rigid and don’t address the unique workflows found in each healthcare environment. In contrast, a custom solution ensures your application is precisely tooled to your organizational goals, regulatory needs, and data management requirements.
But why is this so critical, especially right now? Healthcare has become more data-intensive than ever, with patient medical histories, pharmaceuticals, and insurance billing all converging in highly complex systems. Hospitals are adopting telemedicine solutions, leveraging wearable data, and taking advantage of analytics platforms that predict patient flow or medication efficacy. You might wonder: Where does a custom platform fit into this complex ecosystem?
The answer is that custom platforms can integrate these various data streams into a single, coherent environment. Additionally, it allows you to shape an experience that is convenient, trustworthy, and secure for patients, providers, and administrators. Think of a custom solution as a specialized garment tailored to your exact measurements, whereas a pre-made system is like a one-size-fits-all T-shirt that might not be the perfect fit.
Key Considerations and Use Cases
Before diving into the intricacies of custom healthcare software development, it’s crucial to look at the common uses and the reasons behind them. The following scenarios show where custom systems can make a real difference:
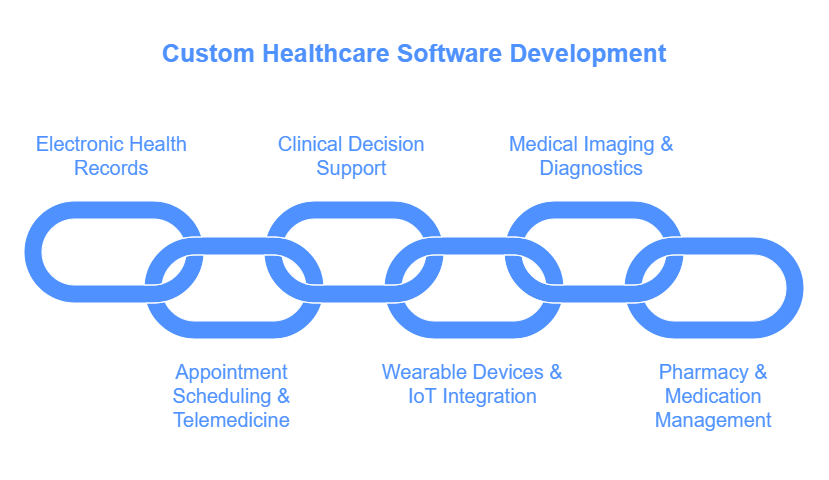
- Electronic Health Records (EHRs)
Many clinics require specialized EHR systems that accommodate unique data fields, incorporate telehealth modules, and integrate directly with insurance databases. - Appointment Scheduling & Telemedicine
Some healthtech startups build scheduling platforms that seamlessly integrate with video conferencing and insurance billing. It’s a vital piece of a broader healthtech software strategy. - Clinical Decision Support
By using advanced data analytics and AI, organizations can assist doctors in diagnosing diseases, identifying drug interactions, and predicting patient outcomes. - Wearable Devices & IoT Integration
Wearable technology is booming, but not all standard platforms sync effortlessly with various brands of smartwatches or health-tracking devices. Custom development fills those gaps by creating unique user interfaces and real-time data dashboards. - Medical Imaging & Diagnostics Platforms
Healthcare organizations often handle high-resolution images and must comply with stringent guidelines for privacy and image storage. Custom solutions ensure that images remain secure but still easily accessible for diagnosis. - Pharmacy & Medication Management
Hospitals and outpatient clinics might need specialized software to track meds, manage allergies, and coordinate with local pharmacies in real time.
Each scenario above demonstrates how custom medical software planning can align specific requirements with your healthtech software strategy. Actually, a one-size-fits-all approach rarely addresses all these aspects with equal effectiveness.
Healthcare Software Development Best Practices
It’s one thing to set out to build healthcare software; it’s another to ensure that your solution remains stable, secure, and compliant. Healthcare software development best practices revolve around the need to protect sensitive data, prevent unauthorized access, and maintain interoperable systems. We’ll delve into some critical considerations below.
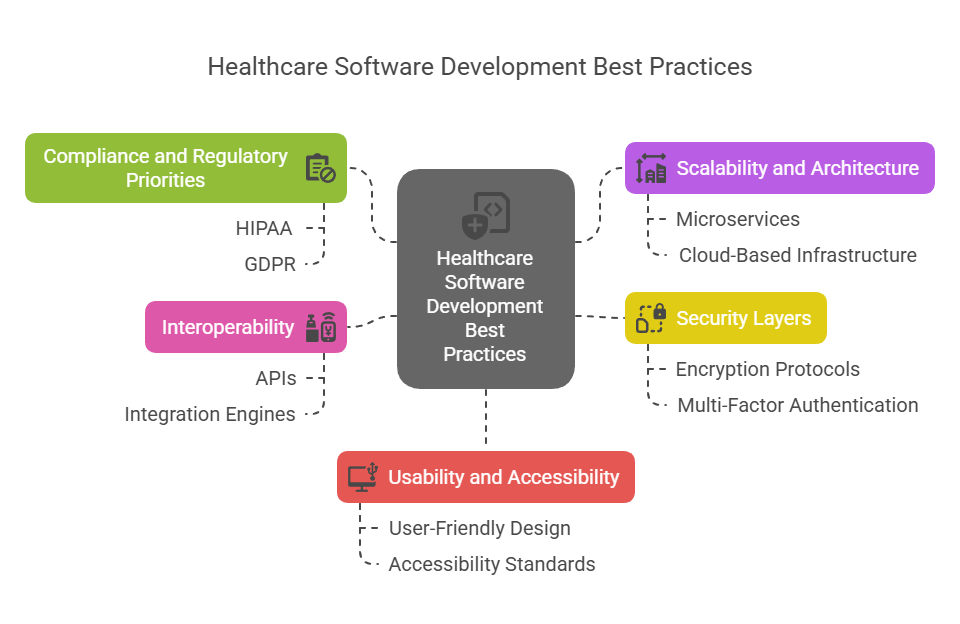
1. Compliance and Regulatory Priorities
Healthcare data is subject to some of the strictest regulations across all industries. In the United States, HIPAA (Health Insurance Portability and Accountability Act) sets the compliance precedent, imposing severe penalties for any mishandling of private patient data. The EU’s GDPR (General Data Protection Regulation) also mandates data protection rules that have broad implications for multinational health organizations. And many regions have local governance (like the UK’s NHS frameworks) that set additional rules.
To keep it simple: you must incorporate encryption (data at rest and in transit), secure login, and proper data auditing. A robust role-based access control (RBAC) structure ensures only authorized personnel can view or update health information. In my experience, paying attention to compliance from the earliest project stages often saves you costly reworks down the line.
2. Scalability and Architecture
Custom efforts in healthtech software strategy should start with an architecture that scales horizontally or vertically as patient loads and data volumes increase. Modern microservices-based designs let you break large applications into smaller independent modules (each can be updated or deployed without forcing a complete system overhaul). Cloud-based infrastructures typically offer elasticity, so your software adapts to usage spikes.
But it’s not just about volume; it’s also about performance. If your hospital sees an influx of patients during flu season, your application should handle heavier workloads and quickly retrieve patient data with minimal downtime.
3. Security Layers
In a world where data breaches can have life-altering consequences, robust security measures are nonnegotiable. Here are some strategies to keep in mind when you build healthcare software:
- Use encryption protocols like TLS for data in transit
- Implement advanced threat detection (alerting on suspicious user patterns)
- Enforce multi-factor authentication for user logins
- Regularly conduct third-party security audits
This layered approach ensures that if one measure is compromised, additional safeguards will be in place to protect critical information.
4. Interoperability
Healthcare providers often rely on numerous existing systems (EHRs, billing platforms, insurance databases). If your custom platform can’t talk to these systems using standard formats (like HL7, FHIR, or DICOM), you’ll run into workflow snags and data silos. Aim for an interoperability-first mindset that leverages APIs, integration engines, or middleware.
5. Usability and Accessibility
Even the most advanced platform won’t be well-received if it’s too cumbersome or confusing. Clinicians and nurses, who typically spend busy shifts navigating multiple systems, need interfaces that simplify tasks. Conduct usability tests with real-world professionals or focus groups. Also consider accessibility guidelines to ensure that your interface accommodates potential visual or motor impairments among end-users or patients.
A Step-by-Step Guide to Build Healthcare Software
Let’s assume you’re leading a team that wants to craft a new telemedicine platform for mental health counseling. The following high-level steps illustrate how to manage custom healthcare software development from concept to deployment (and beyond):
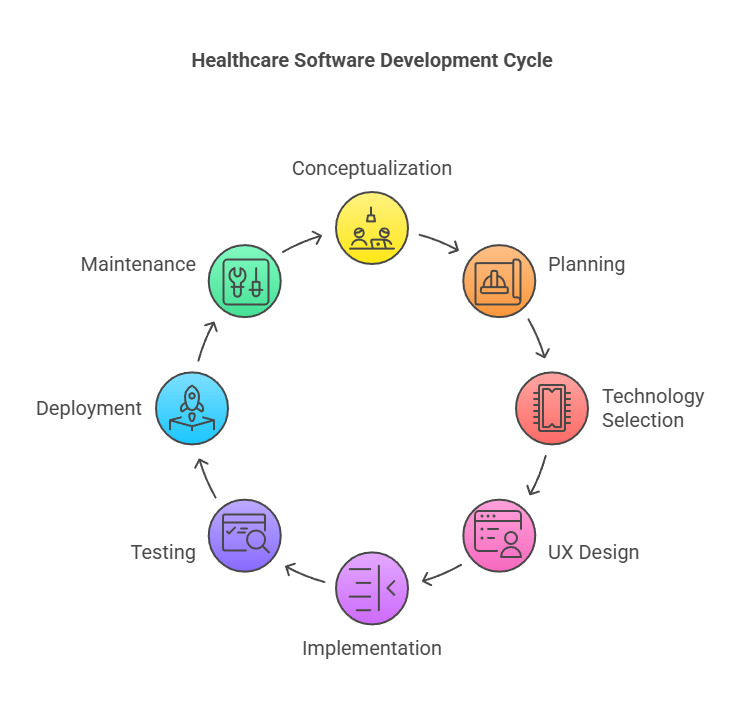
- Conceptualization and Requirements Gathering
– Identify the core problem (e.g., patients needing remote mental health evaluations)
– Align objectives (improved access, better patient-doctor matching)
– Secure stakeholder buy-in (clinicians, patients, insurance partners) - Custom Medical Software Planning
– Document functional requirements (appointment scheduling, secure video calls, chat functionality)
– Outline non-functional requirements (performance, uptime, compliance)
– Allocate budgets and timelines accordingly - Choose Technology Stack and Architecture
– Decide on front-end frameworks (React, Vue) appropriate for your user interface
– Pick back-end technologies (Node.js, Python, Go) suitable for building APIs
– Emphasize modular architectures (microservices) and ensure data encryption from day one - Designing the User Experience
– Create wireframes and prototypes to visualize the platform flow
– Conduct user tests (with mental health counselors and patient volunteers)
– Refine the design based on feedback - Implementation and Integration
– Begin coding modules according to the planned architecture
– Integrate with existing EHR systems or insurance databases if required
– Maintain version control and continuous integration for smooth deployment - Testing and Quality Assurance
– Perform functional tests, load tests, and security assessments
– Verify compliance with HIPAA and other relevant regulations
– Address potential bottlenecks, fix bugs, and retest - Deployment and Training
– Roll out a minimum viable product (MVP) internally for a small subset of real users to gather feedback
– Conduct staff training sessions (for clinicians, support staff, or specialized roles)
– Iterate and refine features based on user responses - Maintenance and Continuous Improvement
– Keep your software updated and regularly patch security vulnerabilities
– Analyze usage data to optimize workflows and predict future enhancements
– Seek ongoing feedback from providers and patients to continually refine your solution
This structured plan not only helps you create a solid foundation but also supports a cycle of continuous improvement.
Common Implementation Challenges and How to Overcome Them
You might wonder, “What if my budget isn’t large enough to handle all these complexities?” The truth is, building or modernizing a healthcare platform can be resource-intensive. However, there are ways to optimize:
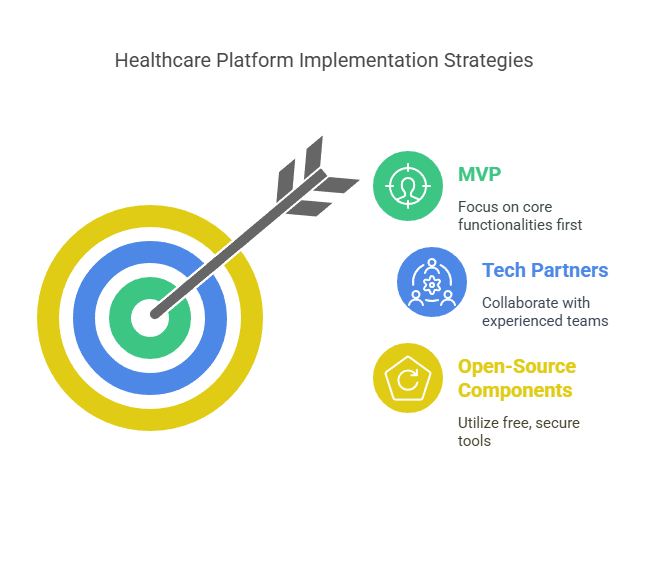
- Start with an MVP: Focus on the core functionalities, then expand.
- Collaboration with Tech Partners: Align with experienced development teams that specialize in healthcare software development best practices.
- Use Open-Source Components: Secure, reputable open-source tools often save on licensing fees and speed up development.
Another challenge is aligning the project’s timeline with compliance audits. The solution? Plan these checks into your project schedule early, so the final launch isn’t delayed. And do not overlook user feedback loops; real-world usage might reveal needs and obstacles you hadn’t anticipated.
But how do you ensure your staff is ready for a new system? Implementation often faces internal resistance. Provide thorough training, demonstrate the benefits, and foster a culture of adaptability. As a side note, encouraging “super-users” or champions from within the clinical team to promote the software can significantly ease adoption.
A Quick Data Table: Key Regulatory Considerations
Security and regulatory needs vary by region, but the table below presents a snapshot of primary regulations you must keep in mind when designing a healthtech software strategy.
| Regulation | Main Focus | Typical Region | Key Requirements |
|---|---|---|---|
| HIPAA | Patient data privacy & security | United States | Encrypt data, ensure access controls, breach notifications |
| GDPR | General data protection | European Union | Lawful processing of data, user consent, data minimization |
| NHS Data Guidelines | Healthcare data management | United Kingdom | Secure patient data handling, staff training, record-keeping |
| PIPEDA | Personal Information Protection Act | Canada | Obtain consent, limit collection, ensure secure storage |
As you can see, these regulatory frameworks shape the entire lifecycle of custom healthcare software development. Neglect them at your peril. Actually, it’s more prudent to integrate compliance checks into your architecture from the get-go.
A Subtle Implementation Detail Most Overlook
Many rushed development projects ignore performance testing under real-world conditions, leading to unexpected crashes or latency issues during peak usage. In healthcare, even a few seconds of system lag can be critical (imagine a surgeon trying to pull up vital medical images). I’d like to refine that statement though: while a few seconds might not always be catastrophic, it can significantly disrupt clinical workflows and erode trust in your platform. Hence, load testing should mirror potential user surges (like during seasonal viral outbreaks) to guarantee the system remains responsive under stress.
Building on Earlier Points: The Importance of User Feedback
Earlier, we touched on testing and training. Let’s expand on that. True success in custom healthcare software development hinges not just on technical excellence, but also on user acceptance. The best practice is to keep your user feedback cycle consistent. That means:
- Running beta tests with frontline clinicians and collecting structured feedback.
- Utilizing analytics tools to pinpoint where users spend the most time or suffer the longest waits in the workflow.
- Incorporating minor revisions and improvements continuously (rather than saving them all for a big annual upgrade).
This incremental approach fosters a sense of shared ownership. When people see their suggestions integrated, they become enthusiastic advocates for the software, championing it to others in their network.
Looking to Build a Digital Healthcare Platform That Scales?
We bring your healthcare software ideas to life—compliantly and efficiently..
Question and Answer: Addressing a Common Concern
Q: You might wonder, “Is it risky to invest in developing custom healthcare software if regulatory requirements keep evolving?”
A: The best way to handle this is to stay proactive. Monitor regulatory changes regularly and design a flexible architecture that can adapt to new rules. Working with experienced healthcare compliance teams or external auditors ensures you’re up to speed on emerging changes, preventing sudden, costly overhauls. If you plan well and keep an eye on the horizon, it’s far less risky than one might assume.
Practical Avenues for Cost Optimization
Building a robust solution can be cost-effective if approached with the right mindset. Here are a few hints:
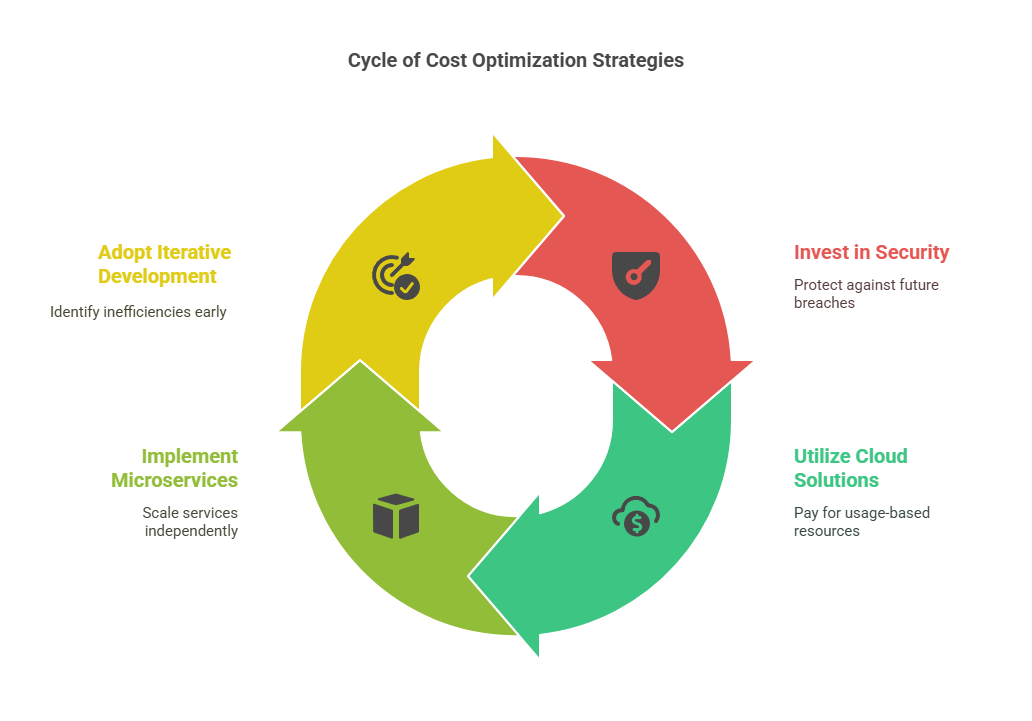
- Aim High on Security
Investing in robust security measures upfront prevents expensive breaches and reputation damage later. - Exploit Cloud Solutions
Cloud-based environments let you pay for server resources on a usage basis instead of buying and maintaining physical servers. - Leverage Microservices
Smaller, independent services can be developed and scaled individually, lowering overhead when specific modules need updates or expansions. - Iterative Development
Break the project into small, manageable sprints. Each sprint yields a working feature, making it easier to spot budget inefficiencies early.
With these strategies, organizations of varying scales can manage their budgets in a sustainable manner, allowing them to build healthcare software that’s both reliable and forward-looking.
Conclusion
Custom healthcare software development sits at the intersection of cutting-edge innovation and the fundamental need to protect patient well-being. By integrating robust security, ensuring regulatory compliance, and focusing on user-centric design, your organization sets the stage for an application that not only meets today’s requirements but also anticipates tomorrow’s challenges. A well-rounded healthtech software strategy can help clinics, hospitals, and health-tech entrepreneurs stay competitive in an evolving market.
When you embrace custom medical software planning with a long-term lens, you gain the flexibility to adapt to new regulations, scale with the changing healthcare landscape, and incorporate emerging technologies (like AI-driven diagnostics or advanced telemedicine features). The ultimate goal? Provide improved patient outcomes, higher efficiency, and streamlined workflows for medical staff.
I encourage you to keep exploring the possibilities, whether that’s diving deeper into healthcare software development best practices or architecting an MVP for your next telehealth service. From compliance to continuous improvement, each step in the process reiterates the importance of thoughtful planning and collaboration. Reach out to expert teams, gather user feedback early, and remain agile in adapting your product roadmap. In doing so, you’ll be well-prepared to build healthcare software that elevates care delivery and transforms the patient experience.




